Cancer Treatment
Radiofrequency Ablation
Radiofrequency Ablation can be used for the treatment of liver or lung cancer. Radiofrequency ablation (RFA) offers a nonsurgical, localized treatment that kills the tumor cells with heat, while sparing the healthy liver or lung tissue. Thus, this treatment is much easier on the patient than systemic therapy. Radiofrequency energy can be given without affecting the patient’s overall health and most people can resume their usual activities in a few days.
In this procedure, the interventional radiologist guides a small needle through the skin into the tumor. From the tip of the needle, radiofrequency energy (similar to microwaves) is transmitted to the tip of the needle, where it produces heat in the tissues. The dead tumor tissue shrinks and slowly forms a scar.
Cryoablation
Recent interventional cryoablation data are showing near 100 percent efficacy for tumors up to four centimeters if localized to the kidney. Larger localized tumors can also be successfully treated with cryoablation depending on size and location
The treatment has an excellent safety profile, and most patients are sent home the same day as the procedure or go home the next day. The most common complication is a bruise (hematoma) around the kidney that goes away by itself.
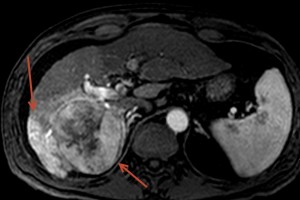
Chemoembolization is a minimally invasive treatment involving targeting infusion of chemotherapy directly in the artery feeding a tumor, most commonly in the liver. Chemoembolization can be used to treat primary liver cancer (Hepatocellular Carcinoma (HCC) or cholangiocarcinoma), as well as metastatic cancer which has spread to the liver from a variety of origins.
Chemoembolization is most commonly used to treat HCC as this type of cancer arises directly from the liver and often does not spread outside the liver. Chemoembolization is extremely effective at treating HCC with tumor responses greater than 70%. The procedure is considered a palliative, not curative, treatment. However, occasionally small tumors are completely killed and do not recur. Patients that develop HCC often have underlying liver cirrhosis and traditional systemic chemotherapy or external beam radiation can injure the liver as much as the tumor, which is how the chemoembolization developed.
The chemotherapeutic drug and type of beads infused into the artery is determined by the tumor type and size. This will be chosen by your doctor during your clinic visit as he/she reviews your history, imaging and labs.
Although primarily used for HCC, chemoembolization has shown promising results in patients with metastatic tumors such as neuroendocrine, colorectal, breast and esophageal cancer.
In small to medium sized tumors, chemoembolization may be combined with radiofrequency ablation (RFA), an ablation technique used to “burn” tumors out. This technique is described above. The combination of these two procedures has been shown to increase the likelihood of complete tumor kill and also prolong survival. If we feel a patient is a candidate for the combination treatment, it will be discussed during the initial clinic visit.
Ultrasound and CT Guided Biopsies
Using imaging guidance, either ultrasound or cat scan, the experts at AVIC can obtain biopsies from nearly any location in the body. Since these procedures are done under close imaging guidance, there is very little risk to the patients. The most commonly biopsied areas are breasts, thyroid gland, lungs, liver, kidneys, and bone marrow.
The PleurX drainage system lets you take control of uncomfortable and painful symptoms from pleural effusions or malignant ascites. A safe, proven option that more than 200,000 patients have used since 1997, the PleurX system helps you drain fluid buildup in the comfort of your own home, without the need for repeat doctor or hospital visits.
- Pleural effusions – fluid buildup around your lungs that makes breathing difficult.
- Malignant ascites – fluid buildup in your abdomen that increases abdominal pressure and discomfort.
How does the PleurX system work?
The PleurX drainage system includes a drainage catheter and drainage bottles that collect fluid. The PleurX catheter is inserted, typically as a simple outpatient procedure, in the chest for draining pleural effusions or in the abdomen for draining malignant ascites. Our experts at AVIC perform this procedure using ultrasound and x-ray guidance. The procedure is done under conscious sedation and takes 30-45 minutes. The end of the catheter stays outside of the body, hidden under a bandage when you are not draining. When you need to drain fluid, simply connect the end of the catheter to the drainage line on the collection bottle, following the directions for use, and the bottle will automatically draw out the fluid.